Kimberly Hrehor (kimberly.hrehor@religroupinc.com) is Program Director and Annie Barnaby is Outreach and Education Specialist at RELI Group Inc. in Catonsville, MD.
How do your billing and/or prescribing submissions compare to those of your peers? Even the most compliant process can benefit from comparisons and analyses of claims, billing, and/or prescribing data. To evaluate these data, develop provider education, and raise awareness of peer claim submission patterns, the Centers for Medicare & Medicaid Services (CMS) initiated the Comparative Billing Report (CBR) program in 2010.
More generally, CMS designed CBRs to protect the Medicare Trust Fund by focusing on areas that may be vulnerable to compliance, billing, and/or prescribing issues.[1] To this end, the CBR team identifies clinical areas with the potential to significantly affect the Medicare Trust Fund, analyzes claims data associated with those areas, and generates individualized CBRs for providers. Each CBR summarizes one provider’s Medicare claims data statistics and offers peer comparison data, making it an educational resource and tool that the provider can use for possible improvement.
What are CBRs?
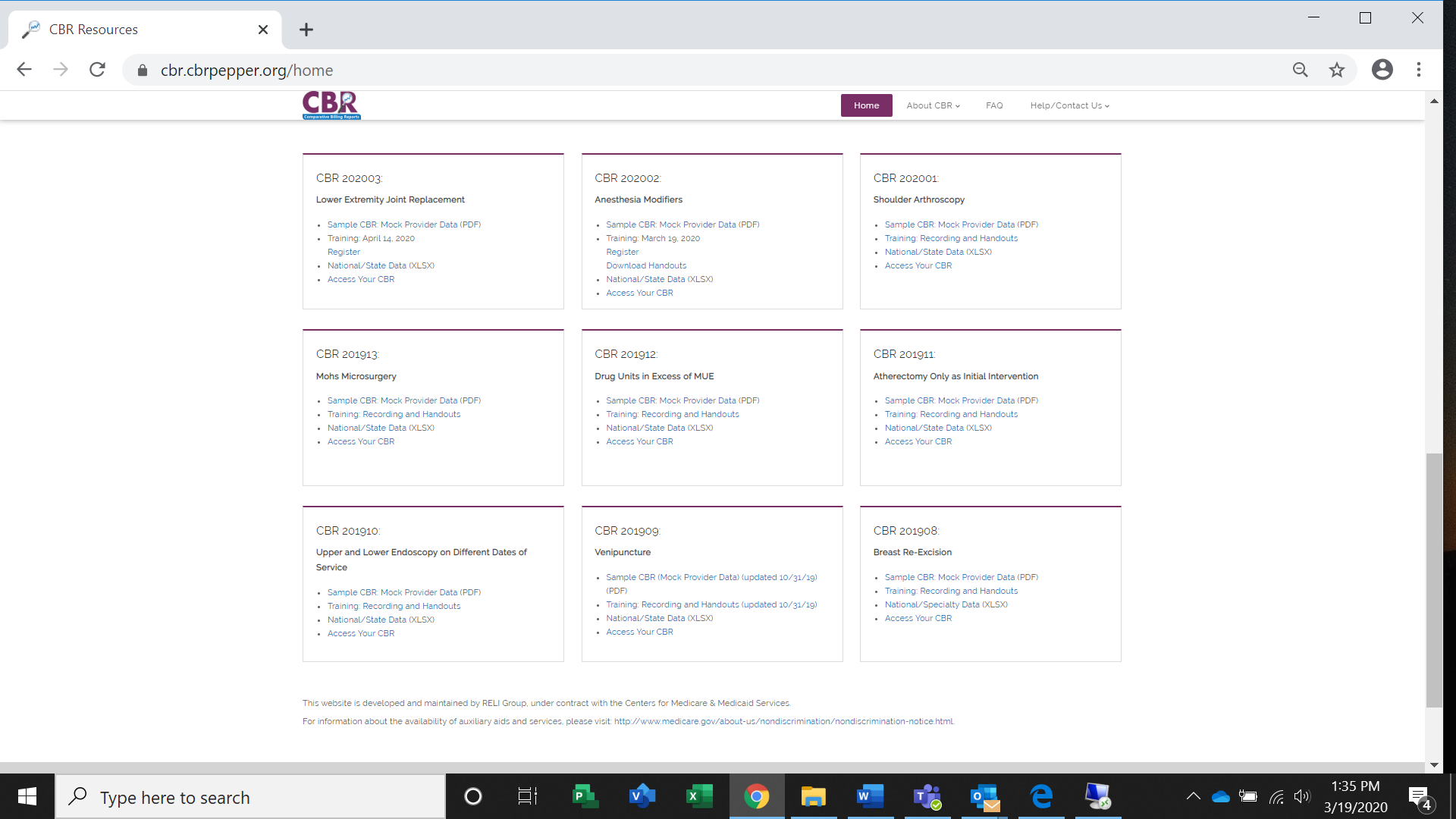
CBRs are free, educational resources for providers that offer complex data in a format that allows providers to compare themselves against their peers on a specialty or state level, as well as on a national level. Each CBR release takes into consideration all providers at a national level to bring attention to potential coding, billing, and/or prescribing vulnerabilities. A CBR summarizes one provider’s Medicare claims data statistics for areas that may be at risk for improper Medicare payments, which may be the result of incorrect coding, incorrect billing, incorrect prescribing, the provision of unnecessary care, and/or nonadherence to Medicare payment policy. Though CBRs cannot identify improper payments, they can alert providers when their claims statistics appear unusual when compared to their peers. After they are released, recent CBRs and their associated resources can be accessed from the homepage of the CBR website (Figure 1) at cbr.cbrpepper.org.
CBRs are designed to be used as educational resources and tools to help providers identify areas for possible improvement in their billing and/or prescribing procedures and compliance plans. The delivery of CBRs supports the integrity of claims submission by summarizing and displaying detailed claims data. The claims data provided in the CBR analyses identify coding, billing, and/or prescribing areas that may be at risk for improper Medicare payments. These analyses and comparisons can detect any outliers in a provider’s billing and/or prescribing processes, which can guide review and verification of compliant claims submission. To help providers with this process, CBRs include information about billing and/or prescribing submissions data and peer comparisons. In addition, CBRs also include information about specific coding guidelines, billing and/or prescribing information, and the connection between compliance and proper billing and/or prescribing.
